The relevance of studying the mechanism of development of chronic prostatitis increases in direct proportion to the increase in the number of diagnosed cases of the disease. It is known that chronic prostatitis (CP) occupies a prominent place among urological diseases and results from many factors integral to modern life (social environment, ecology, increased resistance of pathogens to antibacterial drugs).
Since the disease is not only affecting an increasing percentage of the male population, but is also being diagnosed at younger and younger ages, there is often a rather dismissive attitude towards the problem from doctors whouse model treatment regimens that are incapable of directing to recovery.
What is chronic prostatitis
The diagnosis of chronic prostatitis (CP) combines a fairly wide range of pathological processes in the prostate, manifesting themselves in the form of a chronic inflammatory process in the tissues. However, one cannot speak of CP only because of the penetration of pathogens into the prostate, since such a view justifies attempts to treat prostatitis exclusively with antibiotics, which almost never bring positive resultsdurable.
The main factors underlying the development of pathology can be considered complex changes in the tissues and, accordingly, the functional abilities of the gland, which are the main cause of the development of infectious microflora. Chronic prostatitis, to some extent, is a collective diagnosis that combines several factors:
- Decreased immunity.
- Stagnant processes in the pelvic organs.
- Urodynamic disorder.
- Degenerative processes in the parenchyma of the prostate.
- Trophic disturbance.
- inflammatory processes.
Mechanism of development
The penetration of pathogenic microflora into a healthy prostate gland is practically incapable of causing an inflammatory process, since the prostate microflora has some resistance to pathogens present in the urethra. However, the presence of one or more of the above provoking factors leads to the development of persistent inflammation, accompanied by the appearance of scar formations (fibrotization) or areas of necrosis.
The proliferation of connective tissue in the process of scar formation causes congestive processes in the acini (ducts that provide excretion of secretions), which aggravate the course of the disease. Necrotization of tissues leads to the formation of a cavernous cavity in which, in addition to dead epithelium, a prostatic secret accumulates.
Thus, the main cause of the development of CP is not an infection, but various physiological disorders that allow the inflammatory process to become chronic.
Another distinguishing feature of the disease, which makes diagnosis difficult, isflow periodicity. As a rule, under the influence of external factors or the internal state of the body, there is a periodic change in the intensity of the pathology, during which acute states are replaced by periods of remission.
Often there is not only a complete absence of symptoms, but also the absence of laboratory indicators indicating the presence of an infection (for example, leukocytes). Despite the positive results, this condition cannot be considered a cure, since all physiological disorders of the gland remained unchanged.
The reasons
The main causes of circulatory disorders in the pelvic organs and stagnation of venous blood in the prostate are:
- Permanent stay in a sitting position.
- Hypothermia of the whole body or directly in the pelvic region.
- Systematic constipation.
- Prolonged abstinence from sexual activity or excessive sexual activity.
- The presence in the body of a chronic infection of any localization (sinusitis, bronchitis).
- Excessive physical activity, along with lack of sleep or rest, leads to immune suppression.
- History of urogenital infections (gonorrhea, trichomoniasis).
- Toxic effects on the body due to the systematic use of alcoholic beverages.
The presence of any of these causes leads to the appearance of stagnant processes, a deterioration in the excretory function of the glands, a decrease in cellular resistance to diseases, which contribute to the creation of optimal conditions for the reproduction of microorganismspathogens in the prostate. .
Can chronic prostatitis be cured?
Despite the availability of a large amount of systematized information on the mechanism of CP development,its treatment is extremely difficultand is one of the major problems in modern urological practice.
Due to the fact that the disease progresses in each patient according to an individual pattern, the approach to treatment should also be individual, taking into account all the physiological changes that have occurred in the prostate.
The anatomical features of the prostate, accessible either through the urethra or through the rectum, significantly reduce the effectiveness of the applied therapeutic effect. In this regard, to achieve a relatively stable result, a long course of treatment (usually several months) is required, during which the patient must strictly comply with all the requirements of the doctor.

Unfortunately, a complete cure can only be achievedin 30 out of 100 cases. This is mainly due to an untimely search for medical help, due to a long absence of serious symptoms or a conscious avoidance of unpleasant diagnostic and then therapeutic procedures. As a rule, at the time of treatment, atrophic processes in the prostate are irreversible, and even with long-term treatment it is possible only to completely eliminate the symptoms and achieve a stable remission, the duration of whichdepends on patient compliance. with doctor's recommendations.
Treatment
The complex of measures used in the treatment of CP includes:
Antibacterial therapy
Suppression of the activity of bacterial microflora with the help of antibiotics should be carried out only after a set of laboratory tests, according to the results of which the most effective drug is prescribed.
As a rule, the duration of antibiotics is determined by the severity of the disease and is at least 30 days. It is unacceptable to interrupt treatment, since the remaining microorganisms will become resistant to this group of drugs, and subsequently they will have to be replaced and an even longer course. In the treatment of prostatitis, preference is given to antibiotics that have a bactericidal effect:
- Fluoroquinolones;
- Azalides;
- Aminoglycosides;
- Tetracyclines.

If laboratory tests reveal a specific nature of the infection, for example trichomoniasis or viral origin of prostatitis, nitroimidazoles or an antiviral drug are prescribed in parallel with antibiotics.
The use of antispasmodics and α-blockers
The main purpose of using drugs of this series is to relieve spasms of the pelvic floor, which helps to increase blood supply, improve urine outflow and reduce pain.
Laxatives
In order to avoid excessive stress on the pelvic muscles during the act of defecation, it is advisable to use laxatives, since attempts at constipation can aggravate the patient's condition.
Physiotherapy
One of the most common methods of physiotherapy is rectal prostate massage. The therapeutic effect of the impact of a finger on the prostate, carried out through the anus, is to squeeze out the infected secret, which is then excreted through the urethra.
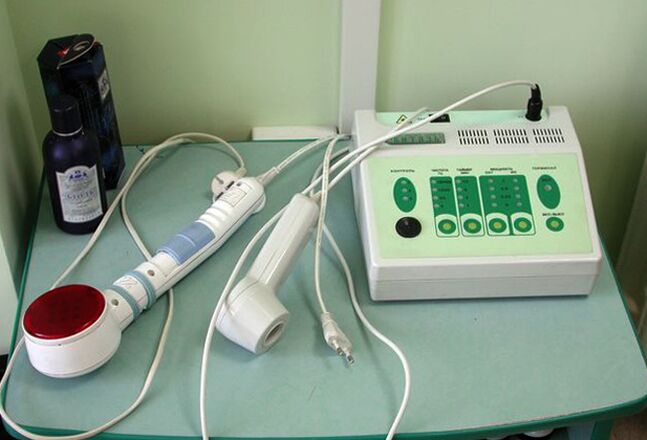
In addition, during massage, the blood supply to the tissues increases, which has a positive effect on antibiotic therapy. To perform rectal prostate massage, the following physiotherapeutic methods are also used:
- Electrical simulator.
- High frequency thermotherapy.
- Infrared laser therapy.
Prevention
After stabilization of the condition, the patient is required to follow the rules that impose certain restrictions on the usual way of life:
- Avoid water procedures in open tanks and swimming pools.
- Get checked regularly by a doctor.
- Completely abstain from drinking alcohol.
- Have a regular sex life with only one partner.
Compliance with the rules will allow you to stay in remission as long as possible and avoid exacerbations of the disease.































